
- AR (Allergic Rhinitis): Allergy of nose
- Sinusitis (Infection of Sinuses)
- DNS (Deviated Nose Septum)
- Epistaxis (Bleeding from nose)
- Rhinoplasty (Reshaping your nose)
AR (Allergic Rhinitis)
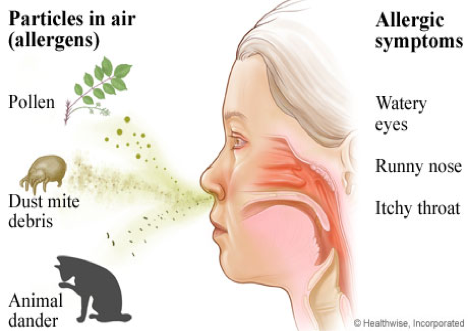
If you sneeze a lot, if your nose is often runny or stuffy, or if your eyes, mouth or nose often feel itchy, you may have allergic rhinitis, a condition that affects 40 million to 60 million Americans.
Allergic rhinitis develops when the body’s immune system becomes sensitized and overreacts to something in the environment that typically causes no problem in most people.
Allergic rhinitis is commonly known as hay fever. But you don’t have to be exposed to hay to have symptoms. And contrary to what the name suggests, you don’t have to have a fever to have hay fever
Allergic rhinitis takes two different forms:
- Seasonal: Symptoms of seasonal allergic rhinitis can occur in spring, summer and early fall. They are usually caused by allergic sensitivity to airborne mold spores or to pollens from grass, trees and weeds.
- Perennial: People with perennial allergic rhinitis experience symptoms year-round. Dust mites, pet hair or dander, cockroaches or mold generally causes it. Underlying or hidden food allergies rarely cause perennial nasal symptoms.
Some people may experience both types of rhinitis, with perennial symptoms getting worse during specific pollen seasons. There are also nonallergic causes for rhinitis including irritants such as cigarette or other smoke, perfumes, cleaning products and other strong odors.
Hay Fever Symptoms
- Runny nose
- Itchy eyes, mouth or skin
- Sneezing
- Stuffy nose due to blockage or congestion
- Fatigue (often reported due to poor quality sleep as a result of nasal obstruction)
Hay Fever Triggers
- Outdoor allergens, such as pollens from grass, trees and weeds
- Indoor allergens, such as pet hair or dander, dust mites and mold
- Irritants, such as cigarette smoke, perfume and diesel exhaust
Hay Fever Management and Treatment
Avoid triggers by making changes to your home and to your behavior.
- Keep windows closed during high pollen periods; use air conditioning in your home and car.
- Wear glasses or sunglasses when outdoors to keep pollen out of your eyes.
- Use “mite-proof” bedding covers to limit exposure to dust mites and a dehumidifier to control mold. (If you smell mildew, you likely have mold).
- Wash your hands after petting any animal and have a nonallergic person help with pet grooming, preferably in a well-ventilated area or outside.
Diagnosing
To find the most effective way to treat allergic rhinitis symptoms, see an allergist Your allergist may start by taking a detailed history, looking for clues in your lifestyle that will help pinpoint the cause of your symptoms. You’ll be asked, among other things, about your work and home environments (including whether you have a pet) your family’s medical history and the frequency and severity of your symptoms.
Sometimes allergic rhinitis can be complicated by several medical conditions, such as a deviated septum (curvature of the bone and cartilage that separate the nostrils) or nasal polyps (abnormal growths inside the nose and sinuses). Any of these conditions will be made worse by catching a cold. Nasal symptoms caused by more than one problem can be difficult to treat, often requiring the cooperation of an allergist and another specialist, such as an otolaryngologist (ear, nose and throat specialist).
Your allergist may recommend a skin test, in which small amounts of suspected allergens are introduced into your skin. Skin testing is the easiest, most sensitive and generally least expensive way of identifying allergens.
Types of skin tests
- Prick or scratch test: In this test, a tiny drop of a possible allergen is pricked or scratched into the skin. Also known as a percutaneous test, this is the most common type of skin test. The results are known within 10 to 20 minutes.
- Intradermal test: A small amount of a possible allergen is injected under the skin using a thin needle. The site is checked for a reaction after about 20 minutes. This test is typically more sensitive than the prick or scratch test.
Management and Treatment
Avoidance
The first approach in managing seasonal or perennial forms of hay fever should be to avoid the allergens that trigger symptoms. Outdoor exposure
- Stay indoors as much as possible when pollen counts are at their peak, usually during the midmorning and early evening (this may vary according to plant pollen), and when wind is blowing pollens around.
- Avoid using window fans that can draw pollens and molds into the house.
- Wear glasses or sunglasses when outdoors to minimize the amount of pollen getting into your eyes.
- ear a pollen mask (such as a NIOSH-rated 95 filter mask) when mowing the lawn, raking leaves or gardening, and take appropriate medication beforehand.
- Don’t hang clothing outdoors to dry; pollen may cling to towels and sheets.
- Try not to rub your eyes; doing so will irritate them and could make your symptoms worse. Indoor exposure
- Keep windows closed, and use air conditioning in your car and home. Make sure to keep your air conditioning unit clean.
- Reduce exposure to dust mites, especially in the bedroom. Use “mite-proof” covers for pillows, comforters and duvets, and mattresses and box springs. Wash your bedding frequently, using hot water (at least 130 degrees Fahrenheit).
- To limit exposure to mold, keep the humidity in your home low (between 30 and 50 percent) and clean your bathrooms, kitchen and basement regularly. Use a dehumidifier, especially in the basement and in other damp, humid places, and empty and clean it often. If mold is visible, clean it with mild detergent and a 5 percent bleach solution as directed by an allergist.
- Clean floors with a damp rag or mop, rather than dry-dusting or sweeping.
Exposure to pets
- Wash your hands immediately after petting any animals; wash your clothes after visiting friends with pets.
- If you are allergic to a household pet, keep the animal out of your home as much as possible. If the pet must be inside, keep it out of the bedroom so you are not exposed to animal allergens while you sleep.
- Close the air ducts to your bedroom if you have forced-air or central heating or cooling. Replace carpeting with hardwood, tile or linoleum, all of which are easier to keep dander-free.
Medications
Many allergens that trigger allergic rhinitis are airborne, so you can’t always avoid them. If your symptoms can’t be well-controlled by simply avoiding triggers, your allergist may recommend medications that reduce nasal congestion, runny nose, sneezing and itching. They are available in many forms — oral tablets, liquid medication, nasal sprays and eyedrops. Some medications may have side effects, so discuss these treatments with your allergist.
Intranasal corticosteroids
Intranasal corticosteroids are the single most effective drug class for treating allergic rhinitis. They can significantly reduce
nasal congestion as well as sneezing, itching and a runny nose.
Talk with your allergist about whether these medications are appropriate and safe for you. These sprays are designed to avoid the side effects that may occur from steroids that are taken by mouth or injection. Take care not to spray the medication against the center portion of the nose (the nasal septum). The most common side effects are local irritation and nasal bleeding. Some older preparations have been shown to have some effect on children’s growth; data about some newer steroids don’t indicate an effect on growth.
Antihistamines
Antihistamines are commonly used to treat allergic rhinitis. These medications counter the effects of histamine, the irritating chemical released within your body when an allergic reaction takes place. Although other chemicals are involved, histamine is primarily responsible for causing the symptoms. Antihistamines are found in eyedrops, nasal sprays and, most commonly, oral tablets and syrup. Antihistamines help to relieve nasal allergy symptoms such as:
- Sneezing and an itchy, runny nose
- Eye itching, burning, tearing and redness
- Itchy skin, hives and eczema
There are dozens of antihistamines; some are available over the counter, while others require a prescription. Patients respond to them in a wide variety of ways.
Generally, the newer (second-generation) products work well and produce only minor side effects. Some people find that an antihistamine becomes less effective as the allergy season worsens or as their allergies change over time. If you find that an antihistamine is becoming less effective, tell your allergist, who may recommend a different type or strength of antihistamine. If you have excessive nasal dryness or thick nasal mucus, consult an allergist before taking antihistamines. Contact your allergist for advice if an antihistamine causes drowsiness or other side effects.
Proper use: Short-acting antihistamines can be taken every four to six hours, while timed-release antihistamines are taken every 12 to 24 hours. The short-acting antihistamines are often most helpful if taken 30 minutes before an anticipated exposure to an allergen (such as at a picnic during ragweed season). Timed-release antihistamines are better suited to long-term use for those who need daily medications. Proper use of these drugs is just as important as their selection. The most effective way to use them is before symptoms develop. A dose taken early can eliminate the need for many later doses to reduce established symptoms. Many times a patient will say that he or she “took one, and it didn’t work.” If the patient had taken the antihistamine regularly for three to four days to build up blood levels of the medication, it might have been effective.
Side effects: Older (first-generation) antihistamines may cause drowsiness or performance impairment, which can lead to accidents and personal injury. Even when these medications are taken only at bedtime, they can still cause considerable impairment the following day, even in people who do not feel drowsy. For this reason, it is important that you do not drive a car or work with dangerous machinery when you take a potentially sedating antihistamine. Some of the newer antihistamines do not cause drowsiness.
A frequent side effect is excessive dryness of the mouth, nose and eyes. Less common side effects include restlessness, nervousness, overexcitability, insomnia, dizziness, headaches, euphoria, fainting, visual disturbances, decreased appetite, nausea, vomiting, abdominal distress, constipation, diarrhea, increased or decreased urination, urinary retention, high or low blood pressure, nightmares (especially in children), sore throat, unusual bleeding or bruising, chest tightness or palpitations. Men with prostate enlargement may encounter urinary problems while on antihistamines. Consult your allergist if these reactions occur.
Important precautions:
- Follow your Doctors instructions.
- Alcohol and tranquilizers increase the sedation side effects of antihistamines.
- Do not use more than one antihistamine at a time, unless prescribed.
- Keep these medications out of the reach of children.
- Know how the medication affects you before working with heavy machinery, driving or doing other performance-intensive tasks; some products can slow your reaction time.
- Some antihistamines appear to be safe to take during pregnancy, but there have not been enough studies to determine the absolute safety of antihistamines in pregnancy. Again, consult your allergist or your obstetrician if you must take antihistamines.
- While antihistamines have been taken safely by millions of people in the last 50 years, don’t take antihistamines before telling your allergist if you are allergic to, or intolerant of, any medicine; are pregnant or intend to become pregnant while using this medication; are breast-feeding; have glaucoma or an enlarged prostate; or are ill.
- Never take anyone else’s medication.
Decongestants
Decongestants help relieve the stuffiness and pressure caused by swollen nasal tissue. They do not contain antihistamines, so they do not cause antihistaminic side effects. They do not relieve other symptoms of allergic rhinitis. Oral decongestants are available as prescription and nonprescription medications and are often found in combination with antihistamines or other medications. It is not uncommon for patients using decongestants to experience insomnia if they take the medication in the afternoon or evening. If this occurs, a dose reduction may be needed. At times, men with prostate enlargement may encounter urinary problems while on decongestants. Patients using medications to manage emotional or behavioral problems should discuss this with their allergist before using decongestants. Patients with high blood pressure or heart disease should check with their allergist before using. Pregnant patients should also check with their allergist before starting decongestants.
Nonprescription decongestant nasal sprays work within minutes and last for hours, but you should not use them for more than a few days at a time unless instructed by your allergist. Prolonged use can cause rhinitis medicamentosa, or rebound swelling of the nasal tissue. Stopping the use of the decongestant nasal spray will cure that swelling, provided that there is no underlying disorder. Oral decongestants are found in many over-the-counter (OTC) and prescription medications, and may be the treatment of choice for nasal congestion. They don’t cause rhinitis medicamentosa but need to be avoided by some patients with high blood pressure. If you have high blood pressure or heart problems, check with your allergist before using them.
Nasal sprays
Nonprescription saline nasal sprays will help counteract symptoms such as dry nasal passages or thick nasal mucus. Unlike decongestant nasal sprays, a saline nasal spray can be used as often as it is needed. Sometimes an allergist may recommend washing (douching) the nasal passage. There are many OTC delivery systems for saline rinses, including neti pots and saline rinse bottles.
Nasal cromolyn blocks the body’s release of allergy-causing substances. It does not work in all patients. The full dose is four times daily, and improvement of symptoms may take several weeks. Nasal cromolyn can help prevent allergic nasal reactions if taken prior to an allergen exposure.
Nasal ipratropium bromide spray can help reduce nasal drainage from allergic rhinitis or some forms of nonallergic rhinitis.
Leukatriene pathway inhibitors
Leukotriene pathway inhibitors (montelukast, zafirlukast and zileuton) block the action of leukotriene, a substance in the body that can cause symptoms of allergic rhinitis. These drugs are also used to treat asthma.
Immunotherapy
Immunotherapy may be recommended for people who don’t respond well to treatment with medications or who experience side effects from medications, who have allergen exposure that is unavoidable or who desire a more permanent solution to their allergies. Immunotherapy can be very effective in controlling allergic symptoms, but it doesn’t help the symptoms produced by nonallergic rhinitis.
Two types of immunotherapy are available: allergy shots and sublingual (under-the-tongue) tablets.
- Allergy shots: A treatment program, which can take three to five years, consists of injections of a diluted allergy extract, administered frequently in increasing doses until a maintenance dose is reached. Then the injection schedule is changed so that the same dose is given with longer intervals between injections. Immunotherapy helps the body build resistance to the effects of the allergen, reduces the intensity of symptoms caused by allergen exposure and sometimes can actually make skin test reactions disappear. As resistance develops over several months, symptoms should improve.
- Sublingual tablets: This type of immunotherapy was approved by the Food and Drug Administration in 2014. Starting several months before allergy season begins, patients dissolve a tablet under the tongue daily. Treatment can continue for as long as three years. Only a few allergens (certain grass and ragweed pollens and house dust mite) can be treated now with this method, but it is a promising therapy for the future.
Eye allergy preparations and eyedrops
Eye allergy preparations may be helpful when the eyes are affected by the same allergens that trigger rhinitis, causing redness, swelling, watery eyes and itching. OTC eyedrops and oral medications are commonly used for short-term relief of some eye allergy symptoms. They may not relieve all symptoms, though, and prolonged use of some of these drops may actually cause your condition to worsen. Prescription eyedrops and oral medications also are used to treat eye allergies. Prescription eyedrops provide both short- and long-term targeted relief of eye allergy symptoms, and can be used to manage them.
Check with your allergist or pharmacist if you are unsure about a specific drug or formula.
Treatments that are not recommended for allergic rhinitis
- Antibiotics: Effective for the treatment of bacterial infections, antibiotics do not affect the course of uncomplicated common colds (a viral infection) and are of no benefit for noninfectious rhinitis, including allergic rhinitis.
- Nasal surgery: Surgery is not a treatment for allergic rhinitis, but it may help if patients have nasal polyps or chronic sinusitis that is not responsive to antibiotics or nasal steroid sprays.
Occupational Rhinitis
If you develop symptoms that resemble those of hay fever and that appear or become more serious at work, you may be suffering from occupational rhinitis.
Occupational rhinitis, or work-related rhinitis, is a condition in which symptoms are triggered or further aggravated by allergens in the workplace. These symptoms can include sneezing, a runny nose and watering eyes. Common triggers include cleaning products, chemical fumes, certain types of dust, and corrosive gases.
If your allergy symptoms appear at work, or seem to get worse there, call your allergist, who can help you identify potential triggers and develop a treatment plan.
FAQs
What is allergic rhinitis?
Allergic rhinitis is an allergic reaction to airborne allergens, like seasonal grass or ragweed pollen or year-round allergens like dust and animal dander. Allergic rhinitis is sometimes called “hay fever,” especially when caused by seasonal allergens. Hay fever shares many of the same symptoms as a common cold, but is not caused by a virus or bacteria. Instead, it is caused by your immune system reacting to allergens you breath into your body.
What is hay fever?
Hey fever is another name for allergic rhinitis, most commonly used to describe a seasonal allergic reaction to pollen such as ragweed. However, the term is often used to refer to nasal allergies caused by any inhaled allergen. Despite the name, hay fever is not necessarily a reaction to hay, and it does not cause a fever.
Is allergic rhinitis contagious?
No. Allergic rhinitis (or hay fever) is caused by your immune system’s response to allergens breathed into your body. It is not caused by a virus or bacteria and is not contagious.
What are hay fever symptoms?
Hay fever, or allergic rhinitis, symptoms are similar to the symptoms of a common cold. Some common symptoms include sneezing, congestion, coughing, sinus pressure, itchy watery eyes, and itchy nose, mouth, and throat, and fatigue. It can be difficult to tell the difference between a cold and hay fever. If you have hay fever, your runny nose will likely have a thin, watery discharge, and, despite the name, you will not have a fever. If you have a cold, you may have a thicker or yellowish discharge from your nose, and may have a low-grade fever. Hay fever symptoms can begin immediately after you are exposed to allergens like House dust mite, pollen or animal dander, and will continue as long as your exposure continues. A cold will most likely begin a day or two after exposure to the virus, and can last a few days to a week.
Sinusitis
Broadly there are two types of sinusitis; based on the duration of the symptoms, these are acute sinusitis and chronic sinusitis
Acute Sinusitis
Overview
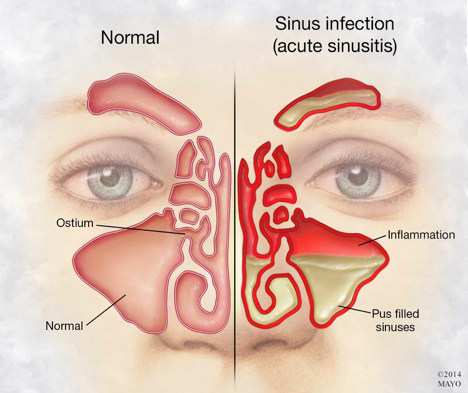
Acute sinusitis (acute rhinosinusitis) causes the cavities around your nasal passages (sinuses) to become inflamed and swollen. This interferes with drainage and causes mucus to build up.
With acute sinusitis, it might be difficult to breathe through your nose. The area around your eyes and face might feel swollen, and you might have throbbing facial pain or a headache.
Acute sinusitis is mostly caused by the common cold. Unless a bacterial infection develops, most cases resolve within a week to 10 days. In most cases, home remedies are all that’s needed to treat acute sinusitis. However, persistent sinusitis can lead to serious infections and other complications. Sinusitis that lasts more than 12 weeks despite medical treatment is called chronic sinusitis.
Symptoms
- Drainage of a thick, yellow or greenish discharge from the nose or down the back of the throat (postnasal drainage)
- Nasal obstruction or congestion, causing difficulty breathing through your nose
- Pain, tenderness, swelling and pressure around your eyes, cheeks, nose or forehead that worsens when bending over Other signs and symptoms can include:
- Ear pressure
- Headache
- Aching in your upper jaw and teeth
- Reduced sense of smell and taste
- Cough, which might be worse at night
- Bad breath (halitosis)
- Fatigue
- Fever
When to see a doctor
Most people with acute sinusitis don’t need to see a doctor.
Contact your doctor if you have any of the following:
- Symptoms that either don’t improve within a few days or worsen
- A persistent fever
A history of recurrent or chronic sinusitis
Causes
Acute sinusitis is most often caused by the common cold, which is a viral infection. In some cases, a bacterial infection develops.
Risk factors
You may be at increased risk of getting sinusitis if you have:
- Hay fever or another allergic condition that affects your sinuses
- A nasal passage abnormality, such as a deviated nasal septum, nasal polyps or tumors
- A medical condition such as cystic fibrosis or an immune system disorder such as HIV/AIDS
Complications
Acute sinusitis complications are uncommon. If they occur, they might include:
- Chronic sinusitis. Acute sinusitis may be a flare-up of a long-term problem known as chronic sinusitis. Chronic sinusitis lasts longer than 12 weeks.
- Meningitis. This infection causes inflammation of the membranes and fluid surrounding your brain and spinal cord.
- Other infections. Uncommonly, infection can spread to the bones (osteomyelitis) or skin (cellulitis).
- Partial or complete loss of sense of smell. Nasal obstruction and inflammation of the nerve for smell (olfactory nerve) can cause temporary or permanent loss of smell.
- Vision problems. If infection spreads to your eye socket, it can cause reduced vision or even blindness that can be permanent.
Prevention
Take these steps to help reduce your risk of getting acute sinusitis:
- Avoid upper respiratory infections. Minimize contact with people who have colds. Wash your hands frequently with soap and water, especially before your meals.
- Manage your allergies. Work with your doctor to keep symptoms under control.
- Avoid cigarette smoke and polluted air. Tobacco smoke and other pollutants can irritate and inflame your lungs and nasal passages. Use a humidifier. If the air in your home is dry, such as it is if you have forced-air heat, adding moisture to the air may help prevent sinusitis. Be sure the humidifier stays clean and free of mold with regular, thorough cleaning.
Diagnosis
Your doctor will feel for tenderness in your nose and face and look inside your nose.
Other methods that might be used to diagnose acute sinusitis and rule out other conditions include:
- Nasal endoscopy. A thin, flexible tube (endoscope) with a fiber-optic light inserted through your nose allows your doctor to visually inspect the inside of your sinuses.
- Imaging studies. A CT scan or MRI can show details of your sinuses and nasal area. While not recommended for uncomplicated acute sinusitis, imaging studies might help identify abnormalities or suspected complications.
- Nasal and sinus cultures. Laboratory tests are generally unnecessary for diagnosing acute sinusitis. However, when the condition fails to respond to treatment or is worsening, tissue cultures might help determine the cause, such as a bacterial infection.
- Allergy testing. If your doctor suspects that allergies have triggered your acute sinusitis, he or she will recommend an allergy skin test. A skin test is safe and quick, and can help pinpoint the allergen that’s responsible for your nasal flare-ups.
Treatment
Most cases of acute sinusitis, those caused by a viral infection, resolve on their own. Self-care techniques are usually all you need to ease symptoms.
Treatments to relieve symptoms
Your doctor may recommend treatments to help relieve sinusitis symptoms, including:
- Saline nasal spray, which you spray into your nose several times a day to rinse your nasal passages.
- Nasal corticosteroids. These nasal sprays help prevent and treat inflammation. Examples include fluticasone (Flonase, Veramyst), budesonide (Rhinocort), mometasone (Nasonex) and beclomethasone (Beconase AQ, Qnasl, others).
- Decongestants. These medications are available in over-the-counter (OTC) and prescription liquids, tablets and nasal sprays. Use nasal decongestants for only a few days. Otherwise they may cause the return of more severe congestion (rebound congestion).
- OTC pain relievers, such as aspirin, acetaminophen (Tylenol, others) or ibuprofen (Advil, Motrin IB, others).
Use caution when giving aspirin to children or teenagers. Children and teenagers recovering from chickenpox or flu-like symptoms should never take aspirin. This is because aspirin has been linked to Reye’s syndrome, a rare but potentially life-threatening condition, in such children.
Antibiotics
Antibiotics usually aren’t needed to treat acute sinusitis. Even if your acute sinusitis is bacterial, it may clear up without treatment.
doctor might wait and watch to see if your bacterial acute sinusitis worsens. However, severe, progressive or persistent symptoms might require antibiotics. If your doctor prescribes an antibiotic, be sure to take the whole course, even after your symptoms get better. If you stop taking them early, your symptoms may recur.
Immunotherapy
If allergies are contributing to your sinusitis, allergy shots (immunotherapy) that help reduce the body’s reaction to specific allergens may help treat your symptoms.
Lifestyle and home remedies
These self-help steps can help relieve sinusitis symptoms:
- Rest. This will help your body fight infection and speed recovery.
- Drink fluids, such as water or juice. This will help dilute mucous secretions and promote drainage. Avoid beverages that contain caffeine or alcohol, as they can be dehydrating. Drinking alcohol can also worsen the swelling of the lining of the sinuses and nose.
- Moisten your sinus cavities. Drape a towel over your head as you breathe in the vapor from a bowl of hot water. Keep the vapor directed toward your face. Or take a hot shower, breathing in the warm, moist air. This will help ease pain and help mucus drain.
- Apply warm compresses to your face. Place warm, damp towels around your nose, cheeks and eyes to ease facial pain.
- Rinse your nasal passages. Use a specially designed squeeze bottle (Sinus Rinse, others) or neti pot. This home remedy, called nasal lavage, can help clear your sinuses.
- If you make your own rinse, use water that’s contaminant-free — distilled, sterile, previously boiled and cooled, or filtered using a filter with an absolute pore size of 1 micron or smaller — to make up the irrigation solution. Also be sure to rinse the irrigation device after each use with contaminant-free water and leave open to air-dry.
- Sleep with your head elevated. This will help your sinuses drain, reducing congestion.
Alternative medicine
No alternative therapies have been proved to ease the symptoms of acute sinusitis, but products containing certain combinations of herbs may help. These combination therapies, sold under brand names such as Sinupret and SinuGuard, contain cowslip, gentian root, elderflower, verbena and sorrel.
Possible side effects include stomach upset, diarrhea and allergic skin reactions.
Preparing for your appointment
When you see your doctor, expect a thorough examination of your sinuses. Here’s information to help you get ready for your appointment.
What you can do
Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment
- Key personal information, including whether you have allergies or asthma and family medical history
- All medications, vitamins or other supplements you take, including the doses
- Questions to ask your doctor
Take a family member or friend along, if possible, to help you remember the information you’re given.
Chronic sinusitis
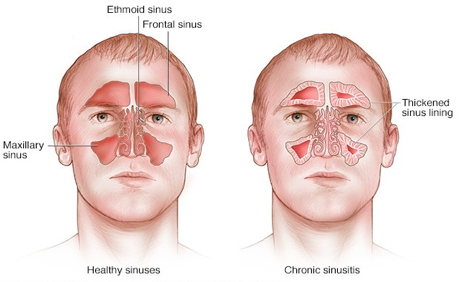
Chronic sinusitis is a common condition in which the cavities around nasal passages (sinuses) become inflamed and swollen for at least 12 weeks, despite treatment attempts.
Also known as chronic rhinosinusitis, this condition interferes with drainage and causes mucus buildup. Breathing through your nose might be difficult. The area around your eyes and face might feel swollen, and you might have facial pain or tenderness.
Chronic sinusitis can be brought on by an infection, by growths in the sinuses (nasal polyps) or by a deviated nasal septum. The condition most commonly affects young and middle-aged adults, but it also can affect children.
Symptoms
At least two of the four primary signs and symptoms of chronic sinusitis must be present with confirmation of nasal inflammation for a diagnosis of the condition. They are:
- Thick, discolored discharge from the nose or drainage down the back of the throat (postnasal drainage)
- Nasal obstruction or congestion, causing difficulty breathing through your nose
- Pain, tenderness and swelling around your eyes, cheeks, nose or forehead
- Reduced sense of smell and taste in adults or cough in children
Other signs and symptoms can include:
- Ear pain
- Aching in your upper jaw and teeth
- Cough that might worsen at night
- Sore throat
- Bad breath (halitosis)
- Fatigue or irritability
- Nausea
Chronic sinusitis and acute sinusitis have similar signs and symptoms, but acute sinusitis is a temporary infection of the sinuses often associated with a cold. The signs and symptoms of chronic sinusitis last longer and often cause more fatigue. Fever isn’t a common sign of chronic sinusitis, but you might have one with acute sinusitis. When to see a doctor
You may have several episodes of acute sinusitis, lasting less than four weeks, before developing chronic sinusitis. You may be referred to an allergist or an ear, nose and throat specialist for evaluation and treatment.
Schedule an appointment with your doctor if:
- You’ve had sinusitis a number of times, and the condition doesn’t respond to treatment
- You have sinusitis symptoms that last more than seven days
- Your symptoms don’t improve after you see your doctor
See a doctor immediately if you have any of the following, which could indicate a serious infection:
- High fever
- Swelling or redness around your eyes
- Severe headache
- Confusion
- Double vision or other vision changes
- Stiff neck
Causes
Common causes of chronic sinusitis include:
- Nasal polyps. These tissue growths can block the nasal passages or sinuses.
- Deviated nasal septum. A crooked septum — the wall between the nostrils — may restrict or block sinus passages.
- Other medical conditions. The complications of cystic fibrosis, gastroesophageal reflux, or HIV and other immune system-related diseases can result in nasal blockage.
- Respiratory tract infections. Infections in your respiratory tract — most commonly colds — can inflame and thicken your sinus membranes and block mucus drainage. These infections can be viral, bacterial or fungal.
- Allergies such as hay fever. Inflammation that occurs with allergies can block your sinuses.
Risk factors
You’re at increased risk of getting chronic or recurrent sinusitis if you have:
- A nasal passage abnormality, such as a deviated nasal septum or nasal polyps
- Asthma, which is highly connected to chronic sinusitis
- Aspirin sensitivity that causes respiratory symptoms
- An immune system disorder, such as HIV/AIDS or cystic fibrosis
- Hay fever or another allergic condition that affects your sinuses
- Regular exposure to pollutants such as cigarette smoke
Complications
Chronic sinusitis complications include:
Meningitis. This infection causes inflammation of the membranes and fluid surrounding your brain and spinal cord.
Other infections. Uncommonly, infection can spread to the bones (osteomyelitis) or skin (cellulitis).
- Partial or complete loss of sense of smell. Nasal obstruction and inflammation of the nerve for smell (olfactory nerve) can cause temporary or permanent loss of smell.
Vision problems. If infection spreads to your eye socket, it can cause reduced vision or even blindness that can be permanent.
Prevention
Take these steps to reduce your risk of getting chronic sinusitis:
Avoid upper respiratory infections. Minimize contact with people who have colds. Wash your hands frequently with soap and water, especially before meals.
Manage your allergies. Work with your doctor to keep symptoms under control.
Avoid cigarette smoke and polluted air. Tobacco smoke and air contaminants can irritate and inflame your lungs and nasal passages. Use a humidifier. If the air in your home is dry, such as it is if you have forced hot air heat, adding moisture to the air may help prevent sinusitis. Be sure to keep the humidifier clean and free of mold with regular, thorough cleaning.
Diagnosis
Your doctor will feel for tenderness in your nose and face and look inside your nose.
Other methods for diagnosing chronic sinusitis include:
Nasal endoscopy. A thin, flexible tube (endoscope) with a fiber-optic light inserted through your nose allows your doctor to see the inside of your sinuses. This also is known as rhinoscopy.
Imaging studies. Images taken using a CT scan or MRI can show details of your sinuses and nasal area. These might pinpoint a deep inflammation or physical obstruction that’s difficult to detect using an endoscope.
Nasal and sinus cultures. Cultures are generally unnecessary for diagnosing chronic sinusitis. However, when the condition fails to respond to treatment or is worsening, tissue cultures might help determine the cause, such as bacteria or fungi.
An allergy test. If your doctor suspects that the condition might be triggered by allergies, he or she might recommend an allergy skin test. A skin test is safe and quick and can help pinpoint the allergen that’s responsible for your nasal flare-ups.
Treatment
The goal of treating chronic sinusitis is to:
- Reduce sinus inflammation
- Keep your nasal passages draining
- Eliminate the underlying cause
- Reduce the number of sinusitis flare-ups
- Treatments to relieve symptoms
- These treatments include:
- Saline nasal irrigation, with nasal sprays or solutions, reduces drainage and rinses away irritants and allergies.
- Nasal corticosteroids. These nasal sprays help prevent and treat inflammation. Examples include fluticasone (Flonase, Veramyst), triamcinolone (Nasacort 24), budesonide (Rhinocort), mometasone (Nasonex) and beclomethasone (Beconase AQ, Qnasl, others). If the sprays aren’t effective enough, your doctor might recommend rinsing with a solution of saline mixed with drops of budesonide (Pulmicort Respules) or using a nasal mist of the solution.
- Oral or injected corticosteroids. These medications are used to relieve inflammation from severe sinusitis, especially if you also have nasal polyps. Oral corticosteroids can cause serious side effects when used long term, so they’re used only to treat severe symptoms.
- Aspirin desensitization treatment, if you have reactions to aspirin that cause sinusitis. Under medical supervision, you’re gradually given larger doses of aspirin to increase your tolerance.
Antibiotics
Antibiotics are sometimes necessary for sinusitis if you have a bacterial infection. If your doctor can’t rule out an underlying infection, he or she might recommend an antibiotic, sometimes with other medications.
Immunotherapy
If allergies are contributing to your sinusitis, allergy shots (immunotherapy) that help reduce the body’s reaction to specific allergens might improve the condition.
Surgery
Endoscopic sinus surgery
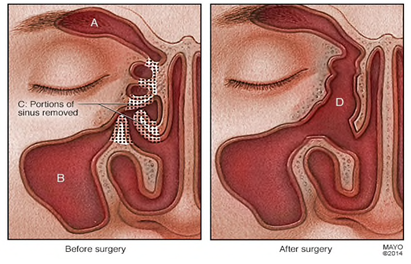
In cases, resistant to treatment or medication, endoscopic sinus surgery might be an option. For this procedure, the doctor uses a thin, flexible tube with an attached light (endoscope) to explore your sinus passages.
Depending on the source of obstruction, the doctor might use various instruments to remove tissue or shave away a polyp that’s causing nasal blockage. Enlarging a narrow sinus opening also may be an option to promote drainage.
Image guided surgery:
The sinuses are physically close to the brain, the eye, and major arteries, always areas of concern when a fiber optic tube is inserted into the sinus region. The growing use of a new technology, image guided endoscopic surgery, is alleviating that concern. This type of surgery may be recommended for severe forms of chronic sinusitis, in cases when previous sinus surgery has altered anatomical landmarks, or where a patient’s sinus anatomy is very unusual, making typical surgery difficult.
Image guidance is a near-three-dimensional mapping system that combines computed tomography (CT) scans and real-time information about the exact position of surgical instruments using infrared signals. In this way, surgeons can navigate their surgical instruments through complex sinus passages and provide surgical relief more precisely. Image guidance uses some of the same stealth principles used by the United States armed forces to guide bombs to their target.
Image guided surgery:
Caldwell Luc operation:
Another option is the Caldwell-Luc operation, which relieves chronic sinusitis by improving the drainage of the maxillary sinus, one of the cavities beneath the eye. The maxillary sinus is entered through the upper jaw above one of the second molar teeth. A “window” is created to connect the maxillary sinus with the nose, thus improving drainage. The operation is named after American physician George Caldwell and French laryngologist Henry Luc and is most often performed when a malignancy is present in the sinus cavity.
Lifestyle and home remedies
These self-help steps can help relieve sinusitis symptoms:
Rest. This will help your body fight inflammation and speed recovery.
Drink fluids, such as water or juice. This will help dilute mucous secretions and promote drainage. Avoid beverages that contain caffeine or alcohol, which can be dehydrating. Drinking alcohol also can worsen the swelling of the lining of the sinuses and nose.
Moisturize your sinus cavities. Drape a towel over your head as you breathe in the vapor from a bowl of medium-hot water. Keep the vapor directed toward your face. Or take a hot shower, breathing in the warm, moist air to help ease pain and help mucus drain.
Apply warm compresses to your face. Place warm, damp towels around your nose, cheeks and eyes to ease facial pain.
Rinse out your nasal passages. Use a specially designed squeeze bottle (Sinus Rinse, others), saline canister or neti pot to rinse your nasal passages. This home remedy, called nasal lavage, can help clear your sinuses.If you make your own rinse, use water that’s contaminant-free — distilled, sterile, previously boiled and cooled, or filtered using a filter with an absolute pore size of 1 micron or smaller — to make up the irrigation solution. Also, be sure to rinse the irrigation device after each use with contaminant-free water, and let air-dry.
Sleep with your head elevated. This will help your sinuses drain, reducing congestion.
DNS (Deviated Nose Septum)
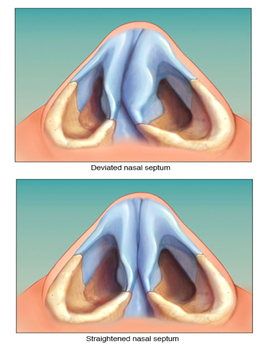
A deviated septum occurs when the thin wall (nasal septum) between your nasal passages is displaced to one side. In many people, the nasal septum is displaced — or deviated — making one nasal passage smaller.
When a deviated septum is severe, it can block one side of your nose and reduce airflow, causing difficulty breathing. The additional exposure of a deviated septum to the drying effect of airflow through the nose may sometimes contribute to crusting or bleeding in certain individuals.
Nasal obstruction can occur from a deviated nasal septum, from swelling of the tissues lining the nose, or from both. Treatment of nasal obstruction may include medications to reduce the swelling or nasal dilators that help open the nasal passages. To correct a deviated septum, surgery is necessary.
Symptoms
Most septal deformities result in no symptoms, and you may not even know you have a deviated septum. Some septal deformities, however, may cause the following signs and symptoms:
- Obstruction of one or both nostrils. This obstruction can make it difficult to breathe through the nostril or nostrils. This may be more noticeable when you have a cold (upper respiratory tract infection) or allergies that can cause your nasal passages to swell and narrow.
- Nosebleeds. The surface of your nasal septum may become dry, increasing your risk of nosebleeds.
- Facial pain. Though there is some debate about the possible nasal causes of facial pain, a severe deviated septum that impacts the inside nasal wall, when on the same side as one-sided facial pain, is sometimes considered a possible cause.
- Noisy breathing during sleep. This can occur in infants and young children with a deviated septum or with swelling of the intranasal tissues.
- Awareness of the nasal cycle. It is normal for the nose to alternate being obstructed on one side, then changing to being obstructed on the other. This is called the nasal cycle. The nasal cycle is a normal phenomenon, but being aware of the nasal cycle is unusual and can be an indication that there is an abnormal amount of nasal obstruction.
- Preference for sleeping on a particular side. Some people may prefer to sleep on a particular side in order to optimize breathing through the nose at night. This can be due to a deviated septum that narrows one nasal passage.
When to see a doctor
See your doctor if you experience:
- A blocked nostril (or nostrils) that doesn’t respond to treatment
- Frequent nosebleeds
- Recurring sinus infections
Causes
A deviated septum occurs when your nasal septum — the thin wall that separates your right and left nasal passages — is displaced to one side.
A deviated septum can be caused by:
- A condition present at birth. In some cases, a deviated septum occurs during fetal development and is apparent at birth.
- Injury to the nose. A deviated septum can also be the result of an injury that causes the nasal septum to be moved out of position.
In infants, such an injury may occur during childbirth. In children and adults, a wide array of accidents may lead to a nose injury and deviated septum — from tripping on a step to colliding with another person on the sidewalk. Trauma to the nose most commonly occurs during contact sports, active play or roughhousing, or automobile accidents.
The normal aging process may affect nasal structures, worsening a deviated septum over time. Also, changes in the amount of swelling of nasal tissues, because of developing rhinitis or rhinosinusitis, can accentuate the narrowing of a nasal passage from a deviated septum, resulting in nasal obstruction.
Risk factors
For some people, a deviated septum is present at birth — occurring during fetal development or due to injury during childbirth. After birth, a deviated septum is most commonly caused by an injury that moves your nasal septum out of place. Risk factors include:
- Playing contact sports
- Not wearing your seat belt while riding in a motorized vehicle
Complications
If you have a severely deviated septum causing nasal obstruction, it can lead to:
- Dry mouth, due to chronic mouth breathing
- A feeling of pressure or congestion in your nasal passages
- Disturbed sleep, due to the unpleasantness of not being able to breathe comfortably through the nose at night
Prevention
You may be able to prevent the injuries to your nose that can cause a deviated septum with these precautions:
- Wear a helmet or a midface mask when playing contact sports, such as football and volleyball.
- Wear a seat belt when riding in a motorized vehicle.
Diagnosis
During your visit, your doctor will first ask about any symptoms you may have.
To examine the inside of your nose, the doctor will use a bright light and sometimes an instrument (nasal speculum) designed to spread open your nostrils. Sometimes the doctor will check farther back in your nose with a long tube-shaped scope with a bright light at the tip. The doctor may also look at your nasal tissues before and after applying a decongestant spray.
Based on this exam, he or she can diagnose a deviated septum and determine the seriousness of your condition.
If your doctor is not an otolaryngologist (ear, nose and throat specialist) and treatment is deemed necessary, you may be referred to a specialist for further consultation and treatment.
Treatment
Managing symptoms
Initial treatment of a deviated septum may be directed at managing the symptoms of the tissues lining the nose, which may then contribute to symptoms of nasal obstruction and drainage. Your doctor may prescribe:
Decongestants. Decongestants are medications that reduce nasal tissue swelling, helping to keep the airways on both sides of your nose open. Decongestants are available as a pill or as a nasal spray. Use nasal sprays with caution, however. Frequent and continued use can create dependency and cause symptoms to be worse (rebound) after you stop using them. Decongestants have a stimulant effect and may cause you to be jittery as well as elevate your blood pressure and heart rate.
Antihistamines. Antihistamines are medications that help prevent allergy symptoms, including obstruction and runny nose. They can also sometimes help nonallergic conditions such as those occurring with a cold. Some antihistamines cause drowsiness and can affect your ability to perform tasks that require physical coordination, such as driving.
Nasal steroid sprays. Prescription nasal corticosteroid sprays can reduce inflammation in your nasal passage and help with obstruction or drainage. It usually takes from one to three weeks for steroid sprays to reach their maximal effect, so it is important to follow your doctor’s directions in using them.
Medications only treat the swollen mucus membranes and won’t correct a deviated septum.
Surgical repair (septoplasty)
If you still experience symptoms despite medical therapy, you may consider surgery to correct your deviated septum (septoplasty). Septoplasty is the usual way to repair a deviated septum. During septoplasty, your nasal septum is straightened and repositioned in the center of your nose. This may require your surgeon to cut and remove parts of your septum before reinserting them in the proper position. The level of improvement you can expect with surgery depends on the severity of your deviation. Symptoms due to the deviated septum — particularly nasal obstruction — often completely resolve. However, any accompanying nasal or sinus conditions affecting the tissues lining your nose — such as allergies — can’t be cured with only surgery.
Epistaxis (Bleeding from nose)

Nosebleeds, also called epistaxes (ep-ih-STAK-seez), involve bleeding from the inside of your nose. Many people have occasional nosebleeds, particularly younger children and older adults.
Although nosebleeds may be scary, they’re generally only a minor annoyance and aren’t dangerous. Nose bleed in children less than 6 years are generally innocuous contrary to those in adults. Frequent nosebleeds are those that occur more than once a week.
Causes
The lining of your nose contains many tiny blood vessels that lie close to the surface and are easily damaged (commonest cause of nose bleeds in children)
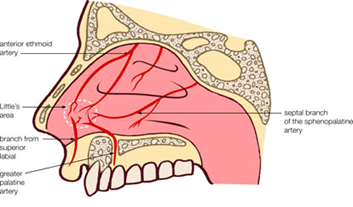
The two most common causes of nosebleeds are:
- Dry air — when your nasal membranes dry out, they’re more susceptible to bleeding and infections
- Nose picking
Other causes of nosebleeds include:
- Acute sinusitis (sinus infection)
- Allergies
- Aspirin use
- Bleeding disorders, such as hemophilia
- Blood thinners (anticoagulants), such as warfarin and heparin
- Chemical irritants, such as ammonia
- Chronic sinusitis
- Cocaine use
- Common cold
- Deviated septum
- Foreign body in the nose
- Nasal sprays, such as those used to treat allergies, if used frequently
- Non-allergic rhinitis (chronic congestion or sneezing not related to allergies)
- Trauma to the nose
Less common causes of nosebleeds include:
- Alcohol use
- Hereditary hemorrhagic telangiectasia
- Idiopathic thrombocytopenic purpura (ITP) & Dengue
- Leukemia
- Nasal and paranasal tumors
- Nasal polyps
- Nasal surgery
- Pregnancy
- Clotting factor/s deficiency
- Tumors eg: Angiofibroma
In general, nosebleeds are not a symptom or result of high blood pressure. It is possible, but rare, that severe high blood pressure may worsen or prolong bleeding if you have a nosebleed (seen in Adults).

When to see a doctor
Most nosebleeds aren’t serious and will stop on their own or by following self-care steps.
Seek emergency medical care if nosebleeds:
- Follow an injury, such as a car accident
- Involve a greater than expected amount of blood
- Interfere with breathing
- Last longer than 30 minutes even with compression
- Occur in children younger than age 2
Don’t drive yourself to an emergency room if you’re losing a lot of blood. Call your local emergency number or have someone drive you. Talk to your doctor if you’re having frequent nosebleeds, even if you can stop them fairly easily. It’s important to determine the cause of frequent nosebleeds.
Self-care steps for occasional nosebleeds include:
- Sit upright and lean forward. By remaining upright, you reduce blood pressure in the veins of your nose. This discourages further bleeding. Sitting forward will help you avoid swallowing blood, which can irritate your stomach.

- Gently blow your nose to clear out any clotted blood. Spray a nasal decongestant in the nose.
- Pinch your nose. Use your thumb and index finger to pinch both nostrils shut, even if only one side is bleeding. Breathe through your mouth. Continue to pinch for five to 10 minutes. This maneuver puts pressure on the bleeding point on the nasal septum and often stops the flow of blood.
- Repeat. If the bleeding doesn’t stop, repeat these steps for up to a total of 15 minutes. After the bleeding has stopped, to keep it from starting again, don’t pick or blow your nose and don’t bend down for several hours. Keep your head higher than the level of your heart.
Tips to help prevent nosebleeds include:
- Keeping the lining of the nose moist. Especially during colder months when air is dry, apply a thin, light coating of petroleum jelly (Vaseline) or antibiotic ointment (bacitracin, Neosporin) with a cotton swab three times a day. Saline nasal spray also can help moisten dry nasal membranes.
- Trimming your child’s fingernails. Keeping fingernails short helps discourage nose picking.
- Using a humidifier. A humidifier will counteract the effects of dry air by adding moisture to the air.
Rhinoplasty (Reshaping your nose)
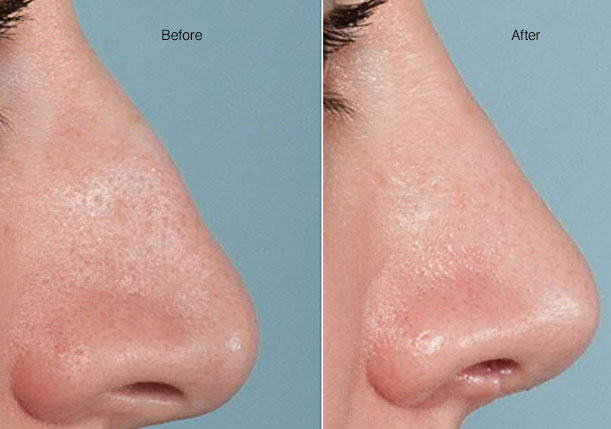
Rhinoplasty (RIE-no-plas-tee) is surgery that changes the shape of the nose. The motivation for rhinoplasty may be to change the appearance of the nose, improve breathing or both.
The upper portion of the structure of the nose is bone, and the lower portion is cartilage. Rhinoplasty can modify bone, cartilage, skin or all three. Talk with your surgeon about whether rhinoplasty is appropriate for you and what it can achieve.
When planning rhinoplasty, your surgeon will consider your other facial features, the skin on your nose and what you would like to change. If you are a candidate for surgery, your surgeon will develop a customized plan for you.
Why it’s done
Rhinoplasty can change the size, shape or proportions of your nose. It may be done to repair deformities from an injury, correct a birth defect or improve some breathing difficulties.
Risks
As with any major surgery, rhinoplasty carries risks such as bleeding, infection and an adverse reaction to the anesthesia. Other possible risks specific to rhinoplasty include:
- Recurring nosebleeds
- Difficulty breathing through your nose
- Permanent numbness in and around your nose
- Possibility of an uneven-looking nose
- Pain, discoloration or swelling that may persist
- Scarring
- Hole in the septum (septal perforation)
Talk to your doctor about how these risks apply to you.
How you prepare
Before scheduling rhinoplasty, you must meet with your surgeon to discuss important factors that determine whether the surgery is likely to work well for you. This meeting generally includes:
- Your medical history. The most important question your doctor will ask you is about your motivation for surgery and your goals. Your doctor will also ask questions about your medical history — including a history of nasal obstruction, surgeries and any medications you take. If you have a bleeding disorder, such as hemophilia, you may not be a candidate for rhinoplasty.
- A physical exam. Your doctor will conduct a complete physical examination, including any laboratory tests, such as blood tests. He or she also will inspect your skin and the inside and outside of your nose. The physical exam helps your doctor determine what changes need to be made and how your physical features — for example, the thickness of your skin or the strength of the cartilage at the end of your nose — may affect your results. The physical exam is also critical for determining the impact of rhinoplasty on your breathing.
- Photographs. Someone from your doctor’s office may take photographs of your nose from different angles. Your surgeon may use computer software to manipulate the photos to show you what kinds of results are possible. Your doctor will use these photos for before-and-after assessments, reference during surgery and long-term reviews. Most importantly, the photos permit a specific discussion about the goals of surgery.
- A discussion of your expectations. You and your doctor should talk about your motivations and expectations. He or she will explain what rhinoplasty can and can’t do for you and what your results might be. It’s normal for people to feel a little self-conscious discussing their appearance, but it’s very important that you’re open with your surgeon about your desires and goals for surgery. Sometimes your surgeon may speak with you about performing a surgery to augment your chin. This is because a small chin will create the illusion of a larger nose. It’s not required to have chin surgery in those circumstances, but it may better balance the facial profile. Once the surgery is scheduled, you’ll need to arrange for someone to drive you home if you’re having an outpatient procedure. For the first few days after anesthesia, you may have lapses of memory, slowed reaction time and impaired judgment. So arrange for a family member or friend to stay with you a night or two to help with personal care tasks as you recover from surgery.
Food and medications
Avoid medications containing aspirin or ibuprofen (Advil, Motrin IB, others) for two weeks before and after surgery. These medications may increase bleeding. Take only those medications approved or prescribed by your surgeon. If you smoke, stop smoking. Smoking slows the healing process after surgery and may make you more likely to get an infection.
What you can expect
Rhinoplasty is not a procedure with a set series of steps. Each operation is unique and is customized for the specific anatomy and goals of the person undergoing the procedure.
Rhinoplasty may be done inside your nose or through a small external incision at the base of your nose, between your nostrils. Your surgeon will likely readjust the bone and cartilage underneath your skin.
Your surgeon can augment your nasal bone or cartilage in several ways, depending on how much needs to be added, the structure of your nose and available materials. For small changes, the surgeon may use cartilage harvested from deeper inside your nose or from your ear. For larger requirements, the surgeon can use cartilage from your rib, implants or bone from other parts of your body.
During the surgery
Rhinoplasty requires local anesthesia with sedation or general anesthesia, depending on the complexity of the surgery and your surgeon’s preferences. Discuss with your doctor beforehand which kind of anesthesia is best in your case.
- Local anesthesia with sedation. This type of anesthesia is usually used in an outpatient setting and is limited to a specific area of your body. Your doctor injects a pain-numbing medication into your nasal tissues and sedates you with medication injected through an intravenous (IV) line. This makes you groggy but not fully asleep.
- General anesthesia. You receive the drug (anesthetic) by inhaling it or through an IV line — a small tube placed in a vein in your hand, neck or chest. General anesthesia affects your entire body and induces a temporary state of unconsciousness. General anesthesia requires a breathing tube.
After the surgery, you’ll be in a recovery room, where the staff monitors your return to wakefulness. You might leave later that day or, if you have other health issues, you might stay overnight.
After the surgery
After the surgery you need to rest in bed with your head raised higher than your chest, to reduce bleeding and swelling. Your nose may be congested because of swelling or from the splints placed inside your nose during surgery.
In most cases, the internal dressings remain in place for one to seven days after surgery. Your doctor also tapes a splint to your nose for protection and support. It’s usually in place for about one week.
Slight bleeding and drainage of mucus and old blood are common for a few days after the surgery or after removing the dressing. Your doctor may place a “drip pad” — a small piece of gauze held in place with tape — under your nose to absorb drainage. Change the gauze as directed by your doctor. Don’t place the drip pad tight against your nose.
To further decrease the chances of bleeding and swelling, your doctor may ask that you follow these precautions for several weeks after surgery:
- Avoid strenuous activities such as aerobics and jogging.
- Take baths instead of showers while you have bandages on your nose.
- Don’t blow your nose.
- Eat high-fiber foods, such as fruits and vegetables, to avoid constipation. Constipation can cause you to strain, putting pressure on the surgery site.
- Avoid extreme facial expressions, such as smiling or laughing.
- Brush your teeth gently to limit movement of your upper lip.
- Wear clothes that fasten in the front; don’t pull clothing, such as shirts or sweaters, over your head.
In addition, don’t rest eyeglasses or sunglasses on your nose for at least four weeks after the surgery, to prevent pressure on your nose. You can use cheek rests, or tape the glasses to your forehead until your nose has healed. Use SPF 30 sunscreen when you’re outside, especially on your nose. Too much sun may cause permanent irregular discoloration in the skin of your nose.
Some temporary swelling or black-and-blue discoloration of your eyelids can occur for two to three weeks after nasal surgery. Swelling of the nose takes longer to resolve. Limiting your dietary sodium will help the swelling go away faster. Don’t put anything such as ice or cold packs on your nose after surgery.
Your nose changes throughout your life whether you have surgery or not. For this reason, it’s difficult to say when you have obtained your “final result.” However, most of the swelling is gone at a year.
Results
Very slight changes to the structure of your nose — often measured in millimeters — can make a large difference in how your nose looks. Most of the time, an experienced surgeon can get results both of you are satisfied with. But in some cases, the slight changes aren’t enough, and you and your surgeon might opt for a second surgery for further refinements. If this is the case, you must wait at least a year for the follow-up surgery, because your nose can undergo changes during this time.
Frequently Asked Questions
How is rhinoplasty different from septoplasty?
Rhinoplasty is a surgery to change the shape of the nose. Because both breathing and the shape of the nose are interrelated, sometimes a rhinoplasty is performed not only to change the way the nose looks but typically it’s also performed to improve nasal breathing too. A septoplasty is a surgery to improve breathing by straightening the wall inside the nose that divides the nasal passages into a right and a left side (nasal septum). When the septum is crooked, it can make it harder to breathe through the nose. A septoplasty is often combined with a rhinoplasty.
Is rhinoplasty a simple operation?
No. Rhinoplasty is one of the most challenging operations there is. This is due to several factors. First, the nose is a complicated three-dimensional shape that is in the middle of the face. Changes made during rhinoplasty are often very small but, when added together, can make a significant difference in the way the nose looks and functions. Because these changes are small, so is the margin for error. Swelling and the placement of local anesthetic in the skin distort the nose during surgery, camouflaging many of the subtle changes made. Rhinoplasty is also not a procedure. In other words, there is no standard plan or set order of steps. Each operation is tailored to the needs of the patient.
Will I need to stay in the hospital?
Nearly everyone who has rhinoplasty is able to safely leave the hospital after surgery. In very rare cases, you may stay in the hospital for one night if you are having a hard time with nausea or have other health problems that need to be monitored.
How long is the recovery period?
Plan to take a week off from work, school or other obligations. You will feel progressively better each day during the first week. By the one week appointment, people usually feel like they are themselves again. After surgery, there will be some swelling. The swelling can take many months to resolve although most people stop noticing it after a couple of months. People are typically back to performing most activities after a week and resuming all activities after two to four weeks.
Are there risks?
All surgeries have risks. Fortunately, the risks for rhinoplasty are small and complications are rare. Your doctor will talk to you about the risks and benefits of surgery in detail before the operation.
Does insurance pay for a rhinoplasty?
Sometimes insurance pays for a rhinoplasty but that depends on the insurance policy. Before scheduling surgery, your doctor’s office will help you obtain prior written authorization from your insurance company. Although this is not a guarantee of coverage, it is the only way to confirm that rhinoplasty is a covered benefit. Sometimes insurance will pay for a part of a nasal surgery but not other parts. In these cases, you can contact the business office to obtain a quote for the operation.
How much does rhinoplasty cost?
The cost of a rhinoplasty depends on several factors. The complexity of the surgery, the surgeon’s training and experience, and geography can all play a part in how much a rhinoplasty costs. At Mayo Clinic, the cost of surgery will be the same regardless of which surgeon you choose.
Is rhinoplasty painful?
Not for most people. At the one day post-operative visit, most people rate their pain between 0-4 out of 10.
Will you pack my nose?
Yes. Packing can be uncomfortable to some patients. You will likely have some soft splints in your nose, however. These splints have a hole in them to make it possible to breathe through them, at least for a few days. These splints are easily removed at the one week visit.
How long will I be bruised?
Bruising is uncommon. If you do have some minor bruising, it typically lasts a week or so.
What should I look for in a surgeon?
Most rhinoplasties are performed by plastic surgeons, facial plastic surgeons or otolaryngologists (ENT). Training and board certification in one of these specialties is a good starting point. You want a surgeon who frequently performs rhinoplasty. You want a surgeon with a good reputation among patients and other doctors. If your surgeon has published numerous papers in the medical literature related to rhinoplasty and is invited to speak at educational conferences, that is one indication that their peers recognize expertise in rhinoplasty.
Make sure that your surgery will be performed in an accredited surgical facility or hospital. You should also feel comfortable with your surgeon. Your surgeon should be able to explain to you in understandable terms what is going to happen during your surgery.
